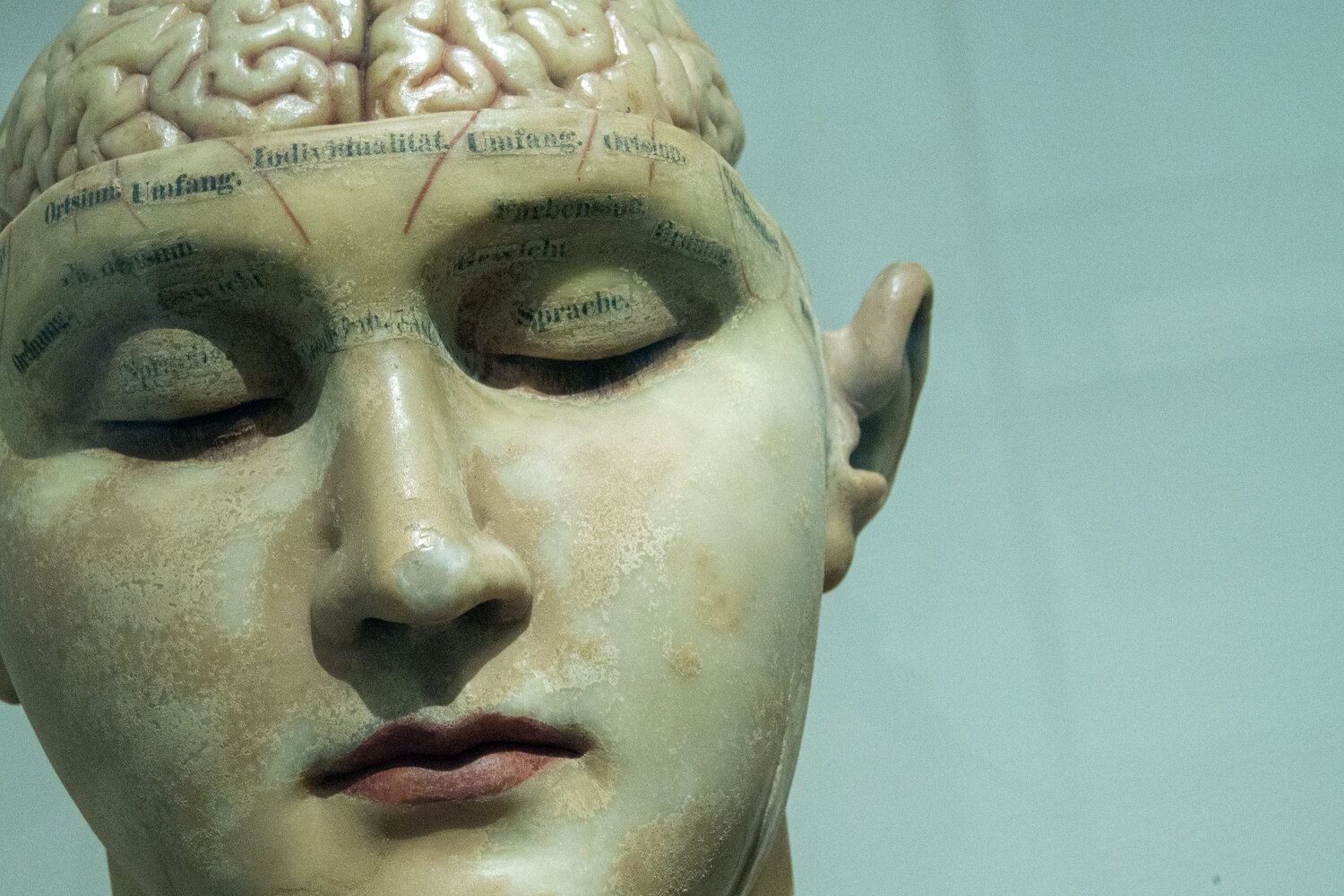
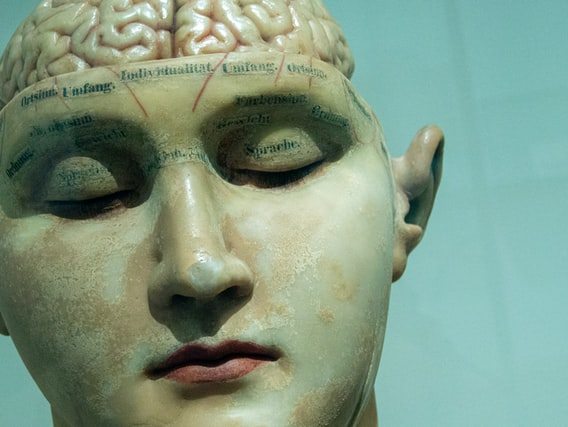
Photo by David Matos on Unsplash
Brain model early 20th century.
Berlin, Germany
Published on NIKON CORPORATION, NIKON D3200
Free to use under the Unsplash License
We live in a world dominated by science, but most people don’t understand its most essential characteristic: establishing standards of evidence to keep us from getting fooled by our own biases and opinions.
- Maintaining standards of evidence is the most important and least appreciated idea in science.
- Modern science was established in the late Renaissance when networks of researchers began working out best practices for linking evidence with conclusions.
- In the face of science denial and attempts to create a post-truth society, we have to protect the primacy of standards of evidence in science and society.
I talk a lot about science to people who are not scientists. It’s generally a lot of fun because most folks are science-curious even if they don’t think about it a lot on their own time. But whether I’m talking about alien life, black holes, or the weirdnesses of quantum mechanics, there is always one really important idea that I try to get across that generally no one is interested in:
Standards of evidence. It’s the most important boring idea in the universe.
Networks of scientists led to scientific societies
The development of modern science was a long, slow process that required input from most of the world’s cultures ranging from ancient Greece and medieval Islam to India and China and eventually Renaissance Europe.
One of the most critical elements in Europe was the gradual build-up of international communities of scholars. While we usually think of science as being driven forward through the inspiration of one singular genius after another, that’s only part of the story. For every Galileo and Newton there were hundreds of people you never heard of. They formed a network of thinkers and tinkerers writing letters to each other and making visits across the continent. In this way, they exchanged notes on things like the best way to carry out an experiment on boiling liquids or a new way to consider the mathematics of problems in celestial mechanics.
Unless you are a scientist, you probably have very little idea of how science knows what it knows, or even more important, how it knows what it doesn’t know.
While they might not have known it at the time, what these scholars were also doing was setting up the foundations for an international order of scientific knowledge that would rest upon mutually agreed standards of evidence.
Eventually these networks became formalized. Scientific academies started popping up in places like Italy where the Academy of the Mysteries of Nature was founded in Naples in 1560. Later the Royal Society in England, formally known as the The Royal Society of London for Improving Natural Knowledge, was established in 1660. The French Academy of Sciences was formed just six years later. Over the years, these institutions and others would lead the way in establishing “best practices” for how to carry out scientific research and how to make sure that the conclusions a scientist drew from that research were supported by the evidence.
Scientific societies led to standards of evidence

Credit: Karlis Reimanis via UnsplashI’m telling you this not because I think the history is so cool (though it is). Instead, what matters is seeing how the idea of standards of evidence was born in its scientific form. It came from people arguing in public over what should count as public facts or better yet public knowledge. Science didn’t drop out of the sky fully formed. It was, and is, the fruit of a very human, very collective effort. The goal of that effort was to determine the best way to ask nature questions and ensure that you’re getting correct answers.
This was not, by the way, a smooth process. There were lots of wrong turns in figuring out what counted as meaningful evidence and what was just another way of getting fooled. But over time, people figured out that there were standards for how to set up an experiment, how to collect data from it, and how to interpret that data. These standards now include things like isolating the experimental apparatus from spurious environmental effects, understanding how data collection devices respond to inputs, and accounting for systematic errors in analyzing the data. There are, of course, many more.
In this way, scientists figured out which standards were useful in linking evidence to conclusions.
Why standards matter
Science is now the most powerful force shaping human life. Without it, there could never be seven billion of us living on the planet at the same time. It has shaped and reshaped how we eat, how we travel, how we deal with sickness, how we communicate, and how we go to war. It is also how we are pushing Earth into new and dangerous (for us) climate states. But despite all this ubiquity and power, unless you are a scientist, you probably have very little idea of how science knows what it knows, or even more important, how it knows what it doesn’t know.
Most of us don’t understand what it means to have standards of evidence or how these standards get applied. That means that we can’t see how the same methods that gave us our cell phones also gave us our understanding of climate change. When a pandemic hits, we can’t see how the science is going to be an evolving process as those standards of evidence get used to sort through the firehose of real-time data. And when it comes to things like UFOs or “Ancient Aliens,” we won’t see that holding fast to those standards is the only thing that can keep us from being fooled by a conclusion that we may want to be true as opposed to accepting the one that actually is true.
Admittedly, standards of evidence is not the most thrilling topic in the world. But it very well may be the most important.
https://bigthink.com/13-8/science-standards-evidence/?utm_term=Autofeed&utm_medium=Social&utm_source88
Zusammenhang Zwischen Zucker Und Hirnerkrankungen
Einem Tübinger Forschungsteam des Instituts für Medizinische Genetik und Angewandte Genomik ist es gelungen, die Bedeutung spezieller Zuckersignale im Körper zu entschlüsseln. Mithilfe der Studienergebnisse können die Wissenschaftler:innen nun neue Ansätze zur Therapie bei Hirnerkrankungen erforschen. Die Studie wurde in der renommierten Fachzeitschrift PNAS (Proceedings of the National Academy of Sciences of the United States of America) publiziert.
Dass zu viel Zucker ungesund ist, predigen Ernährungswissenschaftler:innen bereits seit Jahrzehnten. Als wichtiger Energielieferant für den Körper kommt der Mensch jedoch nicht ganz ohne das Lebensmittel aus. Ob als Energiereserve, zum Muskelerhalt oder zur Förderung der Verdauung – die vielen verschiedenen Kohlehydrate übernehmen im Körper eine Reihe lebenswichtiger Aufgaben.
Ein Internationales Forschungsteam um Dr. Thorsten Schmidt vom Institut für Medizinische Genetik und Angewandte Genomik des Universitätsklinikums Tübingen konnte nun zeigen, dass zu viel Zucker auch in einem ganz anderen Zusammenhang negative Auswirkungen auf die Gesundheit haben kann. Denn Zucker ist nicht gleich Zucker. So versehen Zellen z. B. Eiweiße mit speziellen Zuckermolekülen, um ihre Löslichkeit zu verbessern oder ihre Aktivität zu steuern.
Im Rahmen einer Studie analysierten die Wissenschaftler:innen den Zusammenhang zwischen dem zellulären Mechanismus, durch den Zuckermoleküle an Eiweiß gekoppelt werden und dem Verlauf einer Hirnerkrankung, der sogenannten Spinozerebellaren Ataxie Typ 3. Dr. Thorsten Schmidt, der Leiter der Studie erklärt: „Wir konnten nachweisen, dass diese Zuckersignale in direktem Zusammenhang mit Erkrankungsprozessen im Gehirn stehen, indem wir das dafür verantwortliche Enzym im Körper direkt beeinflussten.“ Dieses Enzym namens O-GlcNAc Transferase (OGT) spielt bei Hirnerkrankungen eine wichtige Rolle: Wurde seine Aktivität vermindert, reduzierten sich auch die Krankheitsfolgen.
Aufgrund dieser Ergebnisse könnte das Enzym OGT ein wichtiger Ansatzpunkt bei der Behandlung von neurologischen Erkrankungen wie Parkinson oder Alzheimer darstellen. „Diese Zuckersignale können tatsächlich als ‚bittersüß‘ bezeichnet werden“, so Dr. Schmidt. „Im Prinzip sind unsere Nervenzellen dringend auf dieses Enzym angewiesen, doch zu viel davon scheint Erkrankungen des Gehirns zu begünstigen.“ Inwieweit die individuelle Ernährung oder geeignete Wirkstoffe diese Zuckersignale und damit auch Hirnerkrankungen beeinflussen können, wird nun in weiteren Studien untersucht. (fa)
Quelle
Pressemitteilung
Pressemitteilung,
Universitätsklinikum Tübingen, Bianca Hermle
Originalpublikation
Pereira Sena P et al.: Pathophysiological interplay between O-GlcNAc transferase and the Machado-Joseph disease protein ataxin-3. Proc Natl Acad Sci U S A. 2021 Nov 23;118 (47): e2025810118. doi: 10.1073/pnas.2025810118. PMID: 34785590.
Foto
David Matos on Unsplash
https://fastenakademie.de/fastenmagazin-ueber-fasten-und-heilfasten/wissenschaft/202-zusammenhang-zwischen-zucker-und-hirnerkrankungen.html
Aantal Nederlanders met een hersenaandoening blijft stijgen
Uit de toekomstverkenning voor 2040 met betrekking tot hersenaandoeningen die het RIVM in 2018 heeft gepubliceerd, kwam een zorgelijke trend naar voren. In het jaar 2040 verwacht het RIVM dat ruim 1 miljoen Nederlanders lijden aan (de gevolgen van) een beroerte, parkinson of dementie.
Een zorgelijk toekomstbeeld
Afgaand op het werkelijk aantal meldingen van deze drie hersenaandoeningen bij de eerstelijnszorgregistratie (NIVEL) over 2021, dan zijn er 372.000 Nederlanders met een beroerte, parkinson en dementie geregistreerd. Dat is al een stijging en als we niets doen worden er dat de komende jaren dus alleen nog maar meer. Een zorgelijk toekomstbeeld, temeer omdat parkinson, dementie en beroerte slechts drie van de honderden hersenaandoeningen zijn die voorkomen. Een hersenaandoening zet het leven van de patiënt en haar naasten volledig op z’n kop. Fysiek, mentaal en sociaal.
https://www.gzpsychologie.nl/aantal-nederlanders-met-een-hersenaandoening-blijft-stijgen/
Glutamaat: belangrijke neurotransmitter voor mentale balans
Voel je je prikkelbaar, angstig of rusteloos? Grote kans dat jouw neurotransmitters niet helemaal in balans zijn, want ze hebben veel invloed op hoe wij ons voelen. In het bijzonder de neurotransmitters glutamaat en GABA. Zij staan in nauwe verbinding met elkaar. Zo werkt glutamaat als een ‘actieve’ neurotransmitter voor het cognitieve vermogen van onze hersenen, zoals ons geheugen. GABA daarentegen is een ‘rustgevende’ neurotransmitter. Als deze balans verstoord is, kunnen we stress ervaren. In dit blogartikel vertellen we je er meer over. Want waar zit glutamaat in? Wat zijn de symptonen van teveel glutamaat en hoe kun je glutamaat verlagen? Daarnaast is onze darmflora een belangrijke speler voor ons zenuwstelsel. Oftewel, glutamaat is een onmisbare schakel voor gezonde hersenen!

Wat is glutamaat?
Glutamaat is een belangrijke neurotransmitter, want het is onmisbaar voor onze informatieverwerking. Daarnaast regelt het ons denk- en leervermogen. Elke neurotransmitter heeft zijn specifieke invloed op onze gesteldheid. Zo zorgt bijvoorbeeld serotonine voor een gelukkig gevoel. Hoe werken neurotransmitters? Via neurotransmitters communiceren onze zenuwcellen (neuronen) met elkaar zodat onze hersenen goed kunnen functioneren. Ze worden aangemaakt uit 20 aminozuren (eiwitten). Zout van glutaminezuur is ook een aminozuur en wordt omgezet in glutamaat. Ons lichaam kan dit aminozuur ook zelf aanmaken.
Glutamaat uit voeding is een belangrijke energiegever dat ons brein gezond houdt, maar waar zit het in? Het is van nature aanwezig in onder andere vlees, vis, kaas, granen en aardappelen. Daarnaast wordt deze neurotransmitter aan voedingsmiddelen toegevoegd als smaakversterker, ook wel bekend als E-621.
Gevaar van glutamaat als E-621
Glutamaat wordt als E-621 of MSG (Mononatriumglutamaat) volop toegevoegd aan verschillende voedingsmiddelen, zoals chips, nootjes, soepen en vleeswaren. Het zorgt voor een intense en hartige smaak, maar ook voor een ‘gelukkig gevoel’. Maar is dat wel echt zo? Jouw hersenen worden namelijk gestimuleerd om door te eten en het geluksgevoel is van korte duur. Hier ligt dan ook het gevaar van dit additief, want het verstoort het natuurlijke verzadigingsgevoel. We krijgen namelijk geen signaal meer door van onze hersenen dat we al genoeg hebben gegeten. Bij overmatig gebruik van E-621 ligt overgewicht dan ook op de loer. Daarnaast kan dit additief gezondheidsklachten geven zoals hoofdpijn, duizeligheid en darmproblemen. Ook is gebleken dat het onze bloedsuikerspiegel en onze hormoonbalans ontregelt.
Herken je de symptonen van een verhoogd glutamaat gehalte? Vermijd deze smaakversterker dan zoveel mogelijk en kies voor pure en verse voeding. Hoewel glutamaat van nature voorkomt in onze voeding, is dus voorzichtigheid geboden bij het kunstmatig additief E-621.

Symptonen van een glutamaat disbalans
Hoewel glutamaat een belangrijke neurotransmitter is, is het echter in een geringe hoeveelheid in ons lichaam aanwezig. Hierdoor kan een verhoogd glutamaat gehalte leiden tot overprikkeling van de zenuwen. Dit kan neurologische problemen geven, zoals hyperactiviteit, rusteloosheid en slapeloosheid. Daarnaast komen prikkelbaarheid, concentratieverlies en angststoornissen veelvuldig voor. Het lichaam bevindt zich dan ook in een stress modus.
De rol van onze darmflora
Wist je dat niet alleen neurotransmitters, maar ook je darmflora bepaalt hoe we ons voelen? Als de darmflora niet optimaal is, kunnen neurotransmitters moeilijker worden aangemaakt. Sombere gevoelens blijken dus niet alleen in de hersenen te ontstaan, maar ook in de darmflora. Via onze darmflora worden signalen afgegeven aan onze hersenen. Heb je last van darmproblemen, zoals constipatie of diarree, dan kan dit leiden tot een tekort aan neurotransmitters. https://liberi.nl/glutamaat/
Is Meningitis Transmissible? What are its Potential Complications?
What is Meningitis?
The inflammation of meninges (of the brain and spinal cord) leads to the development of meningitis. The structure of meninges includes pia mater, arachnoid mater, and dura mater (Hersi, Gonzalez, & Kondamudi, 2020). The meninges line the structures of the spinal cord, brain, and vertebral canal. The term ‘Meningitis’ was coined by John Abercrombie in the year of 2015. Meningitis caused 379,000 deaths worldwide despite the availability of vaccination, treatment, and diagnostic procedures. Meningitis reportedly infected 8.7 million individuals in 2015. The virus or bacterial invasion is the preliminary cause of meningitis and its comorbidities. Meningitis is a serious, debilitating, and life-threatening illness that causes severe disabilities in a variety of clinical scenarios. This condition reportedly causes 25% mortalities on a global scale. Meningitis progresses through a marked elevation in CSF (cerebrospinal fluid) cells (Logan & MacMahon, 2008).
What are the Different Types of Meningitis?
Meningitis is categorized into the following types (CDC, 2020) (Hoffman & Weber, 2009) (Logan & MacMahon, 2008).
1. Bacterial meningitis is the most commonly reported meningitis that progresses through bacterial invasion and warrants prompt medical intervention. The highly aggressive meningitis pathogens include Neisseria meningitidis and Streptococcus pneumoniae. It is a life-threatening condition that could lead to potential clinical complications. Some types of bacterial meningitis could be prevented with the help of vaccines. The clinical differentiation of viral and bacterial meningitis appears infeasible. Eventually, the suspected cases require hospitalizations for diagnostic assessment.
2. Viral meningitis is a less severe form of infection as compared to bacterial meningitis. It progresses through viral invasion and potentially impacts the human immune system. However, individuals with a strong immune system have a greater scope of recovery from viral meningitis. Some of the vaccines claim to prevent a few types of viral meningitis. Lumbar puncture is the only intervention warranted to differentiate between viral and bacterial meningitis. Viral meningitis predominantly impacts young children. However, the disease incidence reduces with age advancement of individuals. Viral meningitis in most of the clinical scenarios develops under the impact of enteroviruses. Despite the self-limiting nature of viral meningitis, the disease has the potential to cause considerable morbidity. Herpes simplex in many cases also leads to the development of viral meningitis. Genital herpes is also a risk factor of viral meningitis. HIV seroconversion increases the risk of meningitis to many folds. The patients infected with viral meningitis without associated encephalitis experience an improvement in their prognostic outcomes.
3. Fungal meningitis is a rare condition that progresses following the inhalation of fungal spores through environmental exposure. The patients affected with HIV, cancer, and diabetes experience a greater predisposition towards fungal meningitis.
4. Parasitic meningitis is a rare condition that develops through the invasion of parasites (other than virus and bacteria).
5. Amebic meningitis or PAM (Primary Amebic Meningoencephalitis) occurs under the impact of Naegleria fowleri following the exposure of high-risk individuals to soil and warm water.
6. Non-infectious meningitis develops as a potential complication of head injury, drug(s) exposure, systemic lupus erythematosus, and cancers.
7. Aseptic meningitis manifests through CSF’s pleocytosis, fever, and meningeal symptoms. However, such type of meningitis is not detected through routine bacterial culture.
8. Mononuclear pleocytosis predominantly develops under the sustained impact of mononuclear cells and WBC (white blood cell count) elevation in the CSF.
9. Meningoencephalitis progresses through the clinical manifestations of parenchymal and meningeal diseases and central nervous system (CNS) infection.
10. Encephalitis establishes through the progressive development of diffuse/focal neurological signs and altered mental status under the impact of cerebral cortex disease and brain parenchyma inflammation.
What are the Potential Causes of Meningitis?
The below-mentioned factors, circumstances, pathogens, medical procedures, and disease conditions potentially elevate the risk of meningitis and its clinical complications (Hersi, Gonzalez, & Kondamudi, 2020).
- Splenectomy
- Sickle cell anemia
- Intravenous medication administration
- Dural defects
- Malignancy/cancers
- Bacterial endocarditis
- VP (ventriculoperitoneal shunt)
- Alcohol use disorder
- Exposure to vectors including ticks and mosquitoes
- Travel across endemic locations
- Exposure to or residence in crowded locations
- Immunocompromised states including AIDS and congenital immunodeficiencies
- Autoimmune disorders
- Organ transplant status
- Iatrogenic conditions based on medical interventions
- Non-adherence to the vaccination schedule
- Age extremes
- Chronic diseases including cystic fibrosis, adrenal insufficiency, diabetes, and liver failure
- Drug reactions
- Paraneoplastic syndromes
- Exposure to Listeria monocytogenes
- Exposure to Haemophilus influenzae
- Exposure to Neisseria meningitidis
- Exposure to group B Streptococcus
- Exposure to Streptococcus pneumoniae
- Exposure to Coccidioides immitis/Coccidiomycosis
- Exposure to Cryptococcus neoformans
- Exposure to close contacts including college dorms and military barracks
- Mucormycosis
- Candidiasis
- Aspergillosis
What are the Clinical Signs and Symptoms of Meningitis?
The clinical presentation of meningitis is based on the following manifestations and/or their varied combinations (Runde & Hafner, 2020).
- Fever
- Neck stiffness or pain
- Photophobia
- Headache
- Dizziness
- Confusion
- Delirium
- Irritability
- Nausea
- Vomiting
- Intracranial pressure elevation
- Seizures
- Neurological deficits
- Altered mental status
- Obtundation
- Focal neurological deficits
- Nuchal rigidity
- Positive Brudzinski’s sign (i.e. involuntary knee flexion following passive neck flexion)
- Positive Kernig’s sign (i.e. hip flexion induced pain in supine position following an extension of the knee)
- Papilledema (fundoscopic finding)
- Purpura fulminans/petechial rash, indicating meningococcal infection
What are the Potential Complications of Bacterial Meningitis?
Bacterial meningitis manifests through the development of high-grade bacteremia that potentially invades CNS and bloodstream (Hoffman & Weber, 2009). The bacteria invade the central nervous system by causing local infection or dural defects, identified through MRI/CCT scans. The research studies have yet to determine the actual anatomical location of bloodstream infection. Some of the experimental studies, however, claim choroid plexus as the location of bacterial invasion. Meningococci infect meninges and choroid plexus; however, the leptomeningeal blood vessels are invaded by pneumococci infiltrate. The evidence-based research literature reveals the highly vascularized anatomical locations as the potential entry points for bacterial invasion (Hoffman & Weber, 2009). The molecular tools of the meningeal pathogens help them to invade CSF barriers based on stringent junctions and complex structures. The Streptococci protein structures encompass the blood-brain barrier following their interaction with phosphorylcholine’s glycoconjugate receptors and eukaryotic cells’ PAF (platelet-activating factor). This eventually triggers endocytosis that leads to the passage of bacterial proteins (including CbpA) through the blood-brain barrier. The integrins and vitronectin interact with the outer membrane protein; however, CD-46 interacts PilC1 adhesin of meningococci (Hoffman & Weber, 2009). The adhesive proteins of Escherichia coli and GBS (group B streptococcal) facilitate their entry into the central nervous system of the newborn babies.
The bacterial invasion progresses through the endothelial cells’ inflammatory activation and ICAM-1 (i.e. adhesion molecular) regulation (Hoffman & Weber, 2009). This episode actively triggers leucocyte invasion that leads to the accumulation of NO (nitric oxide) and MMPs (matrix metalloproteinases) across the CSF/blood-brain barrier. The bacterial invasion, replication, and autolysis across the subarachnoid space unprecedentedly intensify the inflammatory processes. The bacterial invasion also triggers the production of mast cells, perivascular macrophages, and endothelial cells. Interestingly, other than living bacteria, PAMP (pathogen-associated molecular patterns) and the heat-killed bacteria also trigger meningitis in a variety of clinical scenarios. This type of meningitis predominantly occurs under the impact of pathogens including LPS (lipopolysaccharides), PG (peptidoglycan), LTA (lipoteichoic acid), and LP (lipoprotein) (Hoffman & Weber, 2009). The tracking and identification of PAMPs occur through sensors based on immune pattern recognition molecules including LBP and CD14. Similarly, TLR2 recognition occurs through pneumococcal LP and PG. TLR4 plays a predominant role in the signaling of pneumococcal toxin pneumolysin and LPS. MyD88 is an intracellular adaptor protein that channelizes the TLR signals to MAP/NFkB kinases (i.e. inflammatory signaling cascades) that eventually trigger rapid inflammatory responses in the infected patients.
Is Meningitis a Transmissible or Communicable Disease?
- Most forms of bacterial and viral meningitis are communicable or transmitted from one person to another.
- Bacterial meningitis communicates through the throat or respiratory secretions.
- The risk factors for bacterial meningitis transmission include unhygienic conditions, use of unwashed utensils, kissing, sneezing, and coughing (Indiana University, 2019).
- The consumption of contaminated food and contact with feces also greatly increases the risk of meningitis transmission (Davis, 2018).
What are the Diagnostic Measures for Meningitis Assessment?
The following diagnostic interventions are highly warranted to evaluate or rule out the occurrence of bacterial meningitis (Tacon & Flower, 2012).
- Complete blood count assists in evaluating neutrophilia, a predominant marker of infection
- Serum glucose facilitates CSF glucose interpretation
- Creatinine, BUN, and electrolyte levels assist in determining fluid management strategies
- Coagulation profile helps to evaluate potential vascular complications of meningitis
- Blood culture assessments help in tracking 40% to 90% of bacterial meningitis cases
- Inflammatory markers, including procalcitonin and CRP
- CSF lactate
- CSF PCR
- CSF latex agglutination
- Culture and sensitivity (microscopic) study based on gram staining helps to identify the causative organisms including gram-positive cocci (i.e. S. pneumoniae), gram-negative cocci (i.e. N. menigitidis), and gram-negative rod (i.e. H. influenzae)
- CSF-glucose and protein
- CT head assists in evaluating/ruling out meningitis-related conditions including, neurological dysfunction, ICP elevation, focal neurologic complications, infarction, subdural empyema, abscess, and hydrocephalus
- PCR on urine or blood
What are the Treatment Interventions/Approaches for the Clinical Management of Meningitis?
The conservative treatment of meningitis warrants the administration of the below-mentioned pharmacotherapeutic agents based on the age of the patients and/or type of meningitis (Hersi, Gonzalez, & Kondamudi, 2020). s
- Treatment of cryptococcal or fungal meningitis is based on the administration of flucytosine (oral) and amphotericin B (intravenous)
- The meningitis patients allergic to penicillin could be treated with intravenous vancomycin or moxifloxacin
- The patients who develop meningitis due to penetrating trauma or post-procedure foreign body require intravenous vancomycin or meropenem or ceftazidime or cefepime
- The immunocompromised middle-aged adults (of greater than 50 years of age) could receive intravenous ampicillin, or vancomycin, or ceftriaxone for their meningitis management
- The intravenous ceftriaxone and vancomycin appear to be the best treatment option for the clinical management of meningitis in patients between the age group of 18-49 years
- The intravenous ceftriaxone or ampicillin effectively control meningitis manifestations in children above 1 month of age
- Meningitis infected neonates (i.e. below 12 months of age) could be treated through intravenous acyclovir, or gentamycin, or cefepime, or ceftazidime, or cefotaxime or ampicillin
- Ceftriaxone is a 3rd generation cephalosporin that effectively treats gram-negative organisms including Neisseria meningitidis and Streptococcus pneumoniae
- Ceftriaxone has a greater capacity to penetrate CNS as compared to piperacillin-tazobactam
- Ceftriaxone is a treatment of choice for the clinical management of gram-negative sepsis
- Vancomycin effectively treats meningitis related to the invasion of methicillin-resistant Staphylococcus aureus
- Vancomycin is a treatment of choice for the clinical management of meningitis that emanates following the invasion of gram-positive bacteria and resistant pneumococcus
- Ampicillin effectively treats Listeria and other gram-positive bacilli
- Cefepime is a 4th generation cephalosporin having the potential to treat meningitis emanating from pseudomonas invasion
- Cefotaxime is a 3rd generation cephalosporin with a safety profile for neonates
- The clinical management of cerebral perfusion is essentially required for the meningitis patients affected with elevated intracranial pressure (ICP) and related manifestations including bradycardia, non-reactive pupils, neurologic deficits, and altered mental status
- ICP management in meningitis warrants 30 degrees elevation of the patient bed’s head
- ICP management also requires intubation and mild hyperventilation induction
- The pharmacotherapeutic management of ICP warrants the administration of osmotic diuretics including 3% saline and 25% mannitol
- Chemoprophylaxis is highly recommended for the close contacts of a meningitis patient infected with H. influenzae type B and/or Neisseria meningitidis
- The close contacts of meningitis patient (infected with N. meningitidis) require clinical management based on ceftriaxone, or ciprofloxacin, and/or rifampicin
- Rifampicin is the treatment of choice for clinically managing a close contact of the meningitis patient infected with N. meningitidis https://discover.hubpages.com/education/Is-Meningitis-Transmissible-What-are-its-Potential-Complications



