Abstract
Dendritic cells (DCs) are specialized antigen-presenting cells (APCs) that have an unequaled capacity to initiate primary immune responses, including tolerogenic responses. Because of the importance of DCs in the induction and control of immunity, an understanding of their biology is central to the development of potent immunotherapies for cancer, chronic infections, autoimmune disease, and induction of transplantation tolerance. This review discusses recent advances in DC research and the application of this knowledge toward new strategies for the clinical manipulation of DCs for cancer immunotherapy.
Introduction
The concept of tumor “immunosurveillance,” whereby the host immune system is thought to protect against the development of primary cancers, has been debated for decades and has been recently resurrected.1 Evidence in support of tumor immunosurveillance includes observations in mice that lymphocytes and molecules essential for immune function, such as interferon-γ (IFNγ) and perforin, collaborate to protect against the development of certain cancers. Additional corroboration has come from identification of numerous human tumor-associated or tumor-specific antigens recognized by T cells and from isolation of tumor antigen-specific T cells from metastatic lesions. Furthermore, infiltration of certain human cancers by T cells may correlate with dramatically improved survival.2 The accumulating evidence in favor of tumor immunosurveillance indicates that immunotherapies or “vaccines” may prove effective for the treatment of cancer. Indeed, numerous published reports have shown that vaccination of cancer patients with killed tumor cells, tumor cell lysates or tumor antigen proteins, peptides or DNA administered with cytokines or adjuvants can produce immunologic and clinical responses. However, the immune responses to these vaccines are often weak, and clinical responses are rarely complete and long lasting.3–5
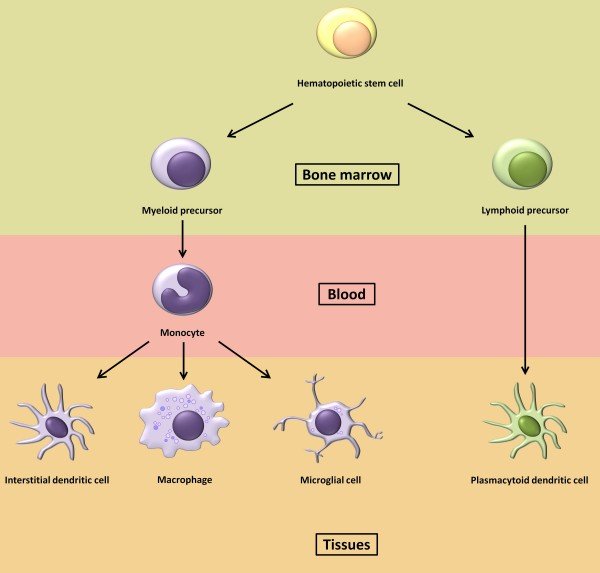
Dendritic cells (DCs) are bone marrow–derived antigen-presenting cells (APCs) that play a critical role in the induction and regulation of immune responses. It has been proposed that the manipulation of DCs as a “natural” vaccine adjuvant may prove to be a particularly effective way to stimulate antitumor immunity.6,7 This hypothesis has been supported by experiments in mice. However, published reports of DC-based vaccine trials in humans have yet to demonstrate improved potency of DC vaccines over more traditional vaccine preparations.5,8,9 In this review we discuss the pitfalls of current DC vaccine approaches in the context of recent advances in DC biology and how improved understanding of DC biology can be applied to develop more effective immunotherapies for cancer.
~ Source http://www.bloodjournal.org/content/104/8/2235?sso-checked=true
